Abstract
Authors:
Alice Baroncini, Nicola Maffulli, Jörg Eschweiler, Friedrich Molsberger, Alexandra Klimuch & Filippo Migliorini
Source : Journal of Orthopaedic Surgery and Research
Background
This Bayesian network meta-analysis investigated the available randomized control trials (RCTs) to point out which acupuncture protocol is the most effective for chronic aspecific low back pain (LBP). Efficacy was measured in terms of pain (Visual Analogic Scale, VAS) and disability (Roland Morris Disability Questionnaire, RMQ), Transcutaneous Electrical Nerve Stimulation (TENS).
Methods
PubMed, Google scholar, Embase, and Scopus were accessed in March 2022. All the RCTs comparing two or more acupuncture modalities for aspecific chronic LBP were accessed. Only studies which investigated the efficacy of acupuncture on patients with symptoms lasting a minimum of 1.5 months, or with at least three episodes in the previous 12 months, were considered eligible. The Review Manager Software (The Nordic Cochrane Collaboration, Copenhagen) was used for the methodological quality assessment. The STATA Software/MP, Version 14.1 (StataCorporation, College Station, Texas, USA), was used for the statistical analyses. The NMA was performed through the STATA routine for Bayesian hierarchical random-effects model analysis.
Results
Data from 44 RCTs (8338 procedures) were retrieved. 56% of patients were women. The mean age of the patients was 48 ± 10.6 years. The mean BMI was 26.3 ± 2.2 kg/m2. The individual group (95% confidence interval (CI) 2.02, 7.98) and the standard combined with TENS (95% CI 2.03, 7.97) demonstrated the highest improvement of the RMQ. The VAS score was lower in the standard combined with TENS group (95% CI 3.28, 4.56). Considering the standard acupuncture group, different studies used similar protocols and acupuncture points and the results could thus be compared. The equation for global linearity did not find any statistically significant inconsistency in any of the network comparison.
Conclusion
Verum acupuncture is more effective than sham treatment for the non-pharmacological management of LBP. Among the verum protocols, individualized acupuncture and standard acupuncture with TENS were the protocols that resulted in the highest improvement in pain and quality of life.
Level of Evidence
Level I, Bayesian network meta-analysis of RCTs.
Introduction
Low back pain (LBP) is common, leading to relevant economic burden [1, 2]. On average, the lifetime prevalence of LBP is as high as 80% [3, 4]. LBP is aspecific in most cases, and no pathoanatomical cause can be found [5]. In such patients, management aims to reduce symptoms and disability, allowing the return to daily life activities and participation in physiotherapy [5]. Current guidelines recommend physiotherapy as a first-line treatment for chronic LBP [6]. As some patients do not experience sufficient benefit from physiotherapy alone, further options are required. Pharmacotherapy is the second step in the management of chronic aspecific LBP [6]. NSAIDs and opiates represent the most successful treatment options [7, 8]. However, potential side-effects of pharmacotherapy, along with the risk of opioids addiction, make this option viable and safe only in the short term. As the number of patients with chronic aspecific LBP increases, so does the demand for safe and effective therapies. Among these, acupuncture has been widely investigated in recent times as possible options, proving to be a safe and effective therapy for chronic aspecific LBP [9,10,11]. Many different acupuncture protocols have been proposed for the management of chronic aspecific LBP. This Bayesian network meta-analysis investigated the available randomized control trials (RCTs) to try and identify which acupuncture protocol is the most effective for chronic aspecific LBP. Efficacy was measured in terms of pain (Visual Analogic Scale, VAS) and disability (Roland Morris Disability Questionnaire, RMQ) to investigate the efficacy of acupuncture on different aspects of the patients’ overall quality of life.
Material and methods
Search strategy
This Bayesian network meta-analysis was conducted according to the PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of healthcare interventions [12]. A guide protocol was preliminary drafted:
- P (population): Chronic low back pain;
- I (intervention): Acupuncture;
- C (comparison): Standardized, sham, individual, auricular, electroacupuncture, acupuncture combined with Transcutaneous Electrical Nerve Stimulation (TENS);
- O (outcomes): VAS, RMQ.
Data source and extraction
Two authors (A.M. and A.B.) independently performed the literature search in April 2022. The following databases were accessed: PubMed, Google scholar, Embase, and Scopus. The following keywords were used in combination: low, lumbar, back, lower, spine, pain, disability, management, therapy, treatments, acupuncture, auricular, tens, electroacupuncture, auricular, individualized, standardized, visual analogic scale, vas, Roland Morris questionnaire. The same authors independently performed the initial screening. If the title and abstract matched the topic, the article full-text was accessed. A cross reference of the bibliographies was also performed. Disagreement was debated and solved by a third author (N.M.).
Eligibility criteria
All the RCTs comparing two or more acupuncture modalities for aspecific chronic LBP were accessed. Only studies which investigated the efficacy of acupuncture on patients with symptoms lasting a minimum of 1.5 months, or with at least three episodes in the previous 12 months were considered eligible. Only studies involving patients aged 18 to 75 were considered. Aspecific LBP was defined as pain that was not arising from a specific pathoanatomical condition [5]. Given the authors language capabilities, articles in English, German, Italian, French and Spanish were eligible. Only level I of evidence studies, according to Oxford Centre of Evidence-Based Medicine [13], were considered. Studies reporting data over acupressure or percutaneous electrical nerve stimulation were not considered. Studies reporting the efficacy of acupuncture in patients with acute pain were not included, nor were those investigating the cervicothoracic segments. Studies investigating patients with neurological deficits were excluded, along with studies including patients with radicular pain (unless the radicular pain was only a minor complaint). Editorials, reviews, letters, opinion, technical notes, comments were not eligible, nor were biomechanical, cadaveric, or animal studies. Only articles reporting quantitative data under the outcomes of interest were considered for inclusion. Missing data under the outcomes of interest warranted exclusion from this study.
Data extraction
Two authors (A.M. and A.B.) independently performed data extraction the resulting articles for inclusion. Study generalities (author, year, journal, design, length of the follow-up) and patient demographic at baseline were extracted (number of samples and related mean BMI and age, percentage of female). For every treatment, the following data were retrieved: VAS, RMQ, adverse events. The groups considered were standard acupuncture alone, standard acupuncture with TENS, electroacupuncture, individualized acupuncture, and auricular acupuncture. The treatment group was classified as individualized acupuncture when the treating physician chose the needling points for each patient, without following a specific protocol. The treatment was defined as standard acupuncture when all patients were treated with the same protocol. Sham acupuncture was defined as the needling of points other than the known acupuncture points: as shallow needling of acupuncture points may also elicit a fibroblast reaction, this method was considered as a form of verum acupuncture [14]. The association of acupuncture with electrostimulation was considered separately.
Risk of bias assessment
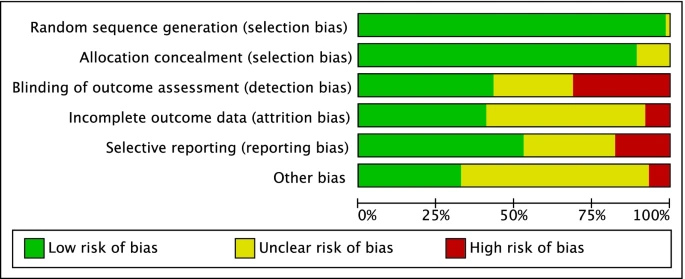
The risk of bias assessment was conducted by two authors (A.M. and A.B.) independently. The Review Manager Software (The Nordic Cochrane Collaboration, Copenhagen) was used for the methodological quality assessment. The following risk of bias were evaluated: selection, detection, reporting, attrition, and other source of bias. For each comparison, the risk of bias was investigated using funnel plots. Plot asymmetries relates to greater risk of bias.
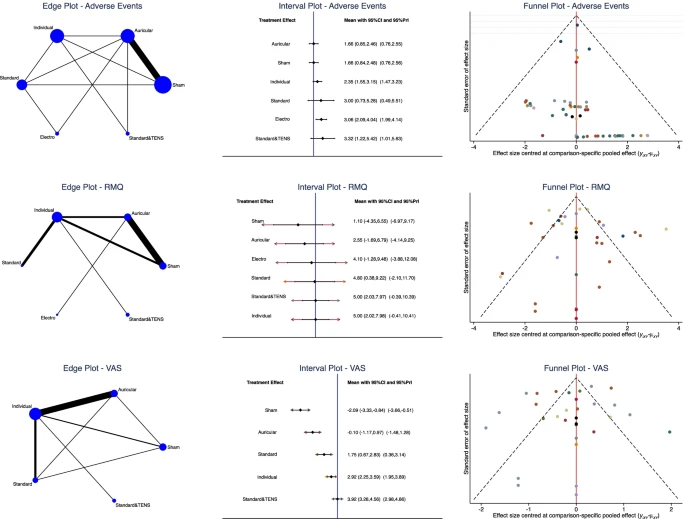
Statistical analysis
The statistical analyses were conducted by the senior author (F.M.). Baseline comparability was assessed through the IBM SPSS software. The analysis of variance (ANOVA) was used for analysis, with P values > 0.1 considered satisfactory. All other treatments rather than standardized, individual, auricular, electroacupuncture, combined with TENS, sham acupuncture were included in the “control group” and excluded from the analysis. The STATA Software/MP, Version 14.1 (StataCorporation, College Station, Texas, USA) was used for the statistical analyses. The NMA was performed through the STATA routine for Bayesian hierarchical random-effects model analysis. The inverse variance method was used for analysis, with standardized mean difference (STD) effect measure. The overall inconsistency was evaluated through the equation for global linearity via the Wald test. If the P value < 0.5, the null hypothesis cannot be rejected, and the consistency assumption could be accepted at the overall level of each treatment. Both confidence (CI) and percentile (PrI) intervals were set at 95%. For each comparison, edge plots were performed to display amount and interpolations of direct comparisons; interval plots were performed to rank the treatments according to their effect measure; and asymmetry of the funnel plots was associated with the greater risk of publication bias.
Results
Search result
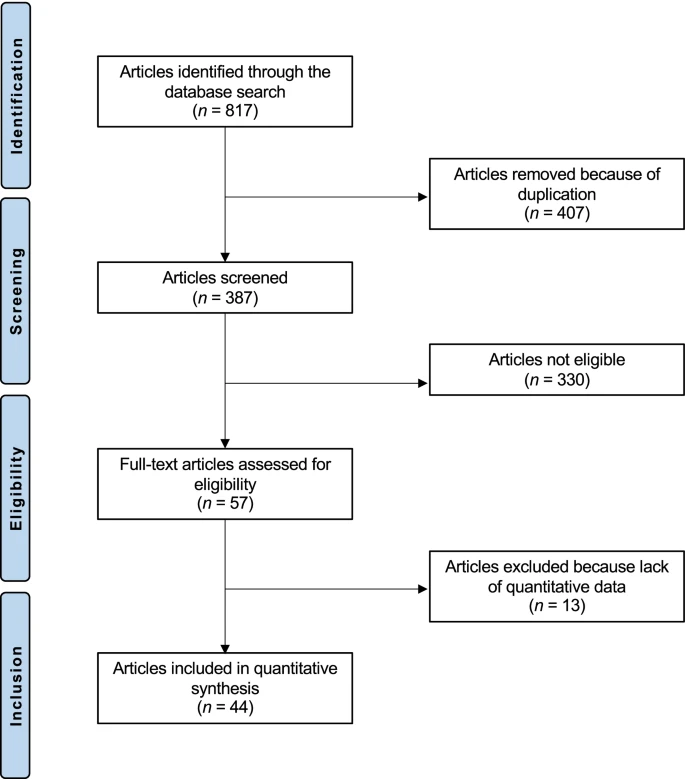
The literature search resulted in 817 RCTs. Four hundred and seven were excluded as they were duplicates. A further 330 studies were incompatible with the eligibility criteria: type of study (N = 89), not matching the topic of interest (N = 193), acupressure or percutaneous electrical nerve stimulation (N = 15), acute LBP (N = 11), concerning cervicothoracic segments (N = 5), presence of severe neurologic impairment or spine deformities (N = 3), acute setting (N = 2), old age (N = 1), language limitations (N = 2), other (N = 9). Another 13 studies were excluded as they did not report quantitative data under the outcomes of interest. This left 44 RCTs for the present study.
Methodological quality assessment
Given the randomized design of the included studies, the risk of selection bias was low. Assessor blinding was performed in 75% (33 of 44) studies; however, the blinding methods were often biased, and the overall risk of detection bias was moderate. The risk of attrition and reporting biases were low to moderate, as was the risk of other bias. Concluding, the methodological quality assessment.
Patient demographics
Data from 8338 procedures were retrieved. 56% of patients were women. The mean age of the patients was 48 ± 10.6 years. The mean BMI was 26.3 ± 2.2 kg/m2. The ANOVA test found moderate baseline comparability in symptoms duration (P > 0.05).
Outcomes of interest
The individual group (SMD 5.00; 95% CI 2.02, 7.98) and the standard combined with TENS (SMD 5.00; 95% CI 2.03, 7.97) demonstrated the highest improvement of RMQ. The VAS score was lower in the standard combined with TENS group (SMD 3.92; 95% CI 3.28, 4.56). Considering the standard acupuncture group, different studies utilized similar protocols and acupuncture points and the results could thus be compared. The equation for global linearity did not find any statistically significant inconsistency in any of the network comparisons.
Discussion
According to the main findings of the present Bayesian network meta-analysis, individualized acupuncture and the standard protocol with TENS may represent the most effective acupuncture strategies for the management of chronic aspecific LBP. These two treatment protocols showed the highest improvements of VAS and RMQ. As verum acupuncture scored better than sham treatment, the present study points to the efficacy of acupuncture in the management of aspecific chronic LBP. This finding further supports current guidelines which recommend acupuncture as one of the possible first-line, non-pharmacological management modality for aspecific chronic LBP [6].
These results are consistent with previous studies [10, 11], which observed a superiority of acupuncture compared to sham treatment [57, 58]. A meta-analysis by Amaral et al. observed only moderate-quality evidence in favor of acupuncture treatment for LBP; however, this study focused only on trigger point acupuncture in the geriatric population, and the results are not directly comparable with those of the present cohort [9]. Nascimiento et al. also observed poor outcomes for acupuncture for LBP in the geriatric population [59]. While no specific characteristics could be highlighted in patients who responded to acupuncture for chronic pain [60], the role of age on the effectiveness of the therapy in the setting of LBP deserves further investigation. A meta-analysis by Mu and colleagues found that acupuncture has only limited effect on pain relief and improvement of the quality of life in the immediate to short term [61]. Li et al. highlighted that a treatment duration of at least 5 weeks is required to achieve 80% of the maximum analgesic effect [62] of acupuncture. Thus, the relatively short timeframe considered by Mu et al. (one to 12 weeks) [61], along with the high risk of bias of the included studies [61], may explain the differences in the observed results. The literature regarding the use of acupuncture in the acute setting is limited and, so far, no studies have been directed to analyze the literature regarding different types of acupuncture for the treatment of acute LBP. Thus, a direct comparison of the presented results with those of the acute setting is not possible. Overall, acupuncture seems to be modestly effective for the management of acute LBP, and the available studies agree that more high-quality work are required to gain more evidence around this topic [63, 64]. Considering the reluctance of many physicians to prescribe acupuncture in patients with chronic LBP, it is fundamental to highlight the efficacy of this treatment in comparison with sham acupuncture. However, the finding that individualized treatment is more effective than standard treatment suggests that a precise diagnosis of chronic LBP according to the criteria of traditional Chinese medicine and the choice of specific acupuncture points may be key for the efficacy of the treatment. This result confirms the clinical experience of the authors. The association of standard protocols with TENS yielded however results similar to those of individualized acupuncture.
This study has several limitations. The most important limitation is the heterogeneous protocols used. Given the randomized design of patient allocation, the risk of selection bias was low. However, some studies did not perform patients or personnel blinding, thus increasing the risk of detection and performance biases, respectively. General health measures were seldom reported, as were also information about the duration of previous symptoms, and type of pain (e.g., central sensitization). Previous conservative strategies were barely reported. Given the lack of quantitative data, the ethnicity of the patients was not analyzed separately. Given the heterogeneity of the protocols used, it was not possible to analyze the effects of the associations of acupuncture with other treatments such as pharmacological management and physio- and psychotherapy. Also, some acupuncture techniques such as moxibustion, cupping or scalp acupuncture were excluded from the study as the available data were not sufficient to grant inclusion. As a multimodal approach is often advisable to tackle the different organic and psychosocial aspects of chronic LBP [6, 65,66,67,68], further studies will be required to investigate the efficacy of different treatment associations and protocols. Furthermore, the available studies only allowed for a precise analysis of the effects of acupuncture in the population < 75 years old: targeted studies for this segment of the population will be required to investigate the efficacy of acupuncture in the elderly.
Conclusion
Verum acupuncture is more efficient than sham treatment for the non-pharmacological management of LBP. Among verum protocols, individualized acupuncture and standard acupuncture with TENS were the protocols that allowed for the highest improvement in pain and quality of life.
Authors:
Alice Baroncini, Nicola Maffulli, Jörg Eschweiler, Friedrich Molsberger, Alexandra Klimuch & Filippo Migliorini

